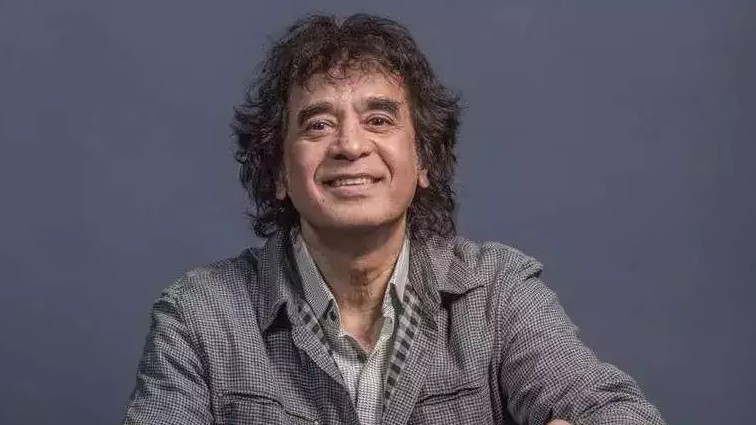
Tabla Maestro Zakir Hussain’s death earlier this week sent shock waves around the world. The multiple-Grammy Award winner reportedly died due to Idiopathic Pulmonary Fibrosis (IPF). Let’s delve into rare disease that claimed the maestro’s life.
IPF is a chronic and progressive lung disease characterized by the development of scar tissue (fibrosis) in the lungs. Over time, this scarring causes the lungs to become stiff, reducing their ability to expand and take in oxygen from the air. This oxygen deficiency limits its transfer to the bloodstream, leading to symptoms such as shortness of breath and fatigue. The condition is termed “idiopathic” because its exact cause remains unknown, although risk factors like smoking, environmental exposures, and genetic predispositions may contribute.
Symptoms
IPF symptoms often develop gradually and worsen over time, making early detection challenging. Key symptoms include:
Progressive shortness of breath: Initially noticeable during physical exertion, this symptom worsens with time and can affect daily activities.
Dry cough: A persistent cough without mucus production is a common early sign.
Fatigue: A constant feeling of tiredness due to the decreased oxygen levels in the body.
Weight loss: Unexplained weight loss is often observed in advanced stages.
Rapid, shallow breathing: Breathing becomes more labored and less efficient as lung function declines.
Chest pain or tightness: Some patients experience discomfort in the chest due to strained lung function.
Loss of appetite: Reduced oxygen levels can lead to general malaise and a diminished desire to eat.
These symptoms significantly impact quality of life, underscoring the importance of early medical intervention.
Diagnosis
Accurate diagnosis of IPF is crucial for initiating timely treatment and improving outcomes. A combination of tests is typically used:
Pulmonary function tests: These measure lung capacity and airflow, helping assess the extent of functional impairment.
Chest X-ray or CT scan: Imaging studies provide detailed views of lung scarring and help differentiate IPF from other lung conditions.
Bronchoscopy: This minimally invasive procedure allows doctors to examine the airways and collect samples for analysis.
Lung biopsy: In some cases, a small tissue sample is obtained for microscopic examination to confirm fibrosis and rule out other diseases.
Early diagnosis can be challenging as symptoms overlap with those of other respiratory conditions, such as asthma or chronic obstructive pulmonary disease (COPD). Therefore, it is essential for individuals experiencing persistent respiratory symptoms to seek medical evaluation promptly.
Treatment of IPF
Although there is no cure for IPF, various treatment options can help manage symptoms, slow disease progression, and improve quality of life:
Medications: Anti-fibrotic drugs, such as pirfenidone and nintedanib, have shown promise in slowing the progression of lung scarring. These medications require regular monitoring for side effects and effectiveness.
Pulmonary rehabilitation: This program combines exercise, education, and counseling to enhance lung function, stamina, and overall well-being.
Home oxygen therapy: Depending on the severity of the condition, supplemental oxygen may be needed to maintain adequate blood oxygen levels and alleviate symptoms.
Lung transplant: For patients with advanced IPF who meet eligibility criteria, a lung transplant can offer a significant improvement in quality of life and survival. However, it involves rigorous evaluation and long-term post-transplant care.
Timely and personalized treatment plans are critical to managing the disease effectively.
Early intervention
Recognizing the symptoms of IPF and seeking prompt medical attention can significantly impact disease management and prognosis. Early diagnosis allows for timely intervention with treatments that may slow disease progression and improve the patient’s quality of life.
While living with IPF is undoubtedly challenging, advancements in medical therapies and a comprehensive approach to care provide hope for better outcomes. With the support of healthcare professionals, caregivers, and the community, individuals with IPF can focus on creating meaningful experiences and enjoying the moments that matter most.
Living with IPF
Adjusting to life with IPF can be challenging, but several strategies can help improve the quality of life and emotional well-being of patients:
Medical management: Regular follow-ups with a pulmonologist and adherence to prescribed treatments are essential for managing symptoms and monitoring disease progression.
Lifestyle modifications: Avoiding smoking, environmental pollutants, and respiratory infections can prevent exacerbations and support lung health.
Support groups: Joining a support group can provide emotional encouragement and connect patients with others facing similar challenges. Sharing experiences and coping strategies can be immensely beneficial.
Mental health support: Living with a chronic condition can take a toll on mental health. Counseling or therapy may help address anxiety, depression, or stress associated with the disease.
By maintaining a positive outlook and actively participating in their care, patients can lead fulfilling lives despite the limitations imposed by IPF.
(Dr. Sulaiman Ladhani, Pulmonologist at Wockhardt Hospitals, Mumbai Central)